Meniscal Injuries
Meniscal Injuries
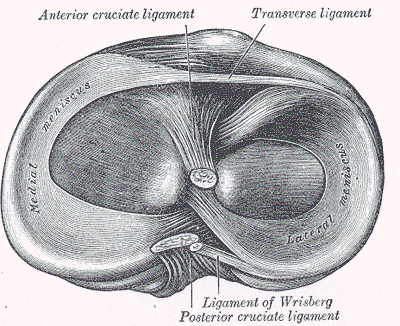
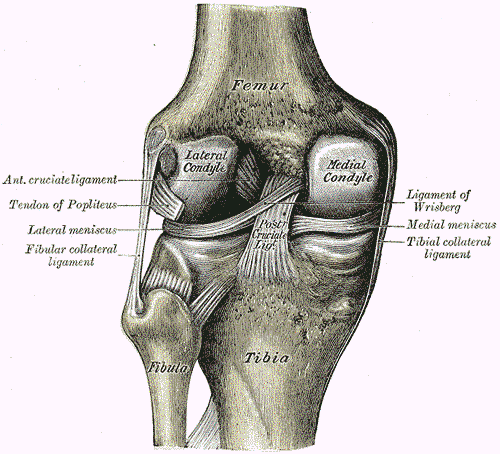
The medial and lateral menisci are two important shock-absorbing structures preserving the health, integrity, and functionality of the knee. Their role is to serve as a cushion between femur and tibia and protect the underlying articular cartilage from being damaged by high-intensity vertical forces. Additionally, menisci increase the contact surface between femur and tibia, distribute stress across the knee during weight bearing tasks, stabilize and facilitate joint movement.
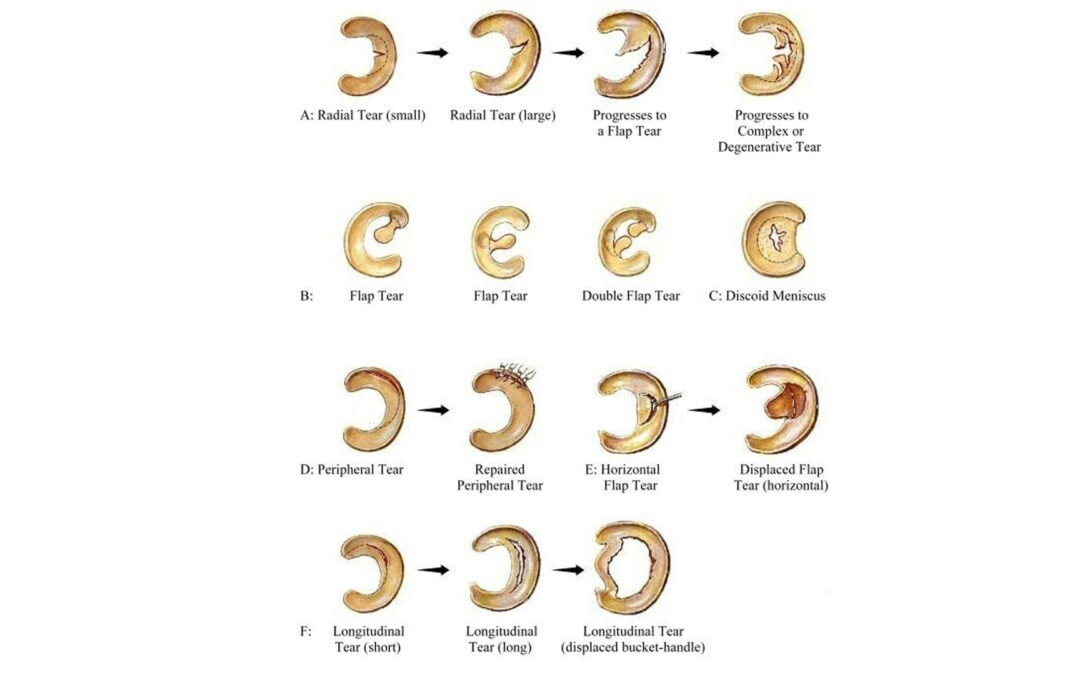
Menisci can be torn or completely ruptured, and the severity of the injury will impact on recovery and outcome. Below there are some examples of the most common meniscal tears:
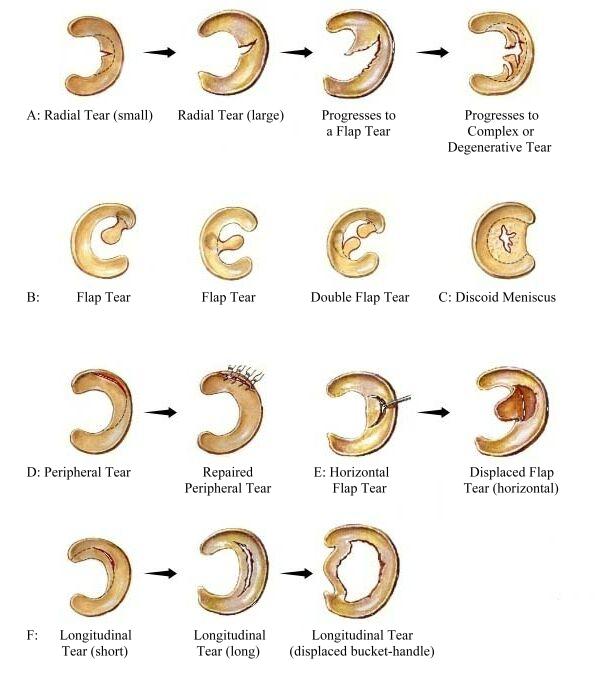
Meniscal injuries can be classified in two main categories: TRAUMATIC and DEGENERATIVE.
Traumatic Meniscal Injury
What is it?
Traumatic meniscal injury often occurs in younger age groups. Most of these individuals are sport athletes below 40 years of age who have sustained a specific trauma in their knee, especially if they play contact sports. The most common traumatic event resulting in meniscal tear is a twisting movement on a semi-flexed, weight bearing knee. Injured people are usually unable to continue to play on after the trauma. Physiotherapists must always screen for the ligaments and, in particular, the anterior cruciate ligament as this can often get damaged by the same trauma. Traumatic meniscal injury is 5 times more common in males than females, because males are more involved in aggressive sporting. Depending on what meniscus is injured, the pain can be located either on the medial or lateral aspect of the knee. Posterior knee pain can often be present, and it is common when the tear is localised on the posterior horn of the meniscus. Common symptoms associated with a traumatic meniscal injury are locking, swelling and giving way of the knee.
What is the management?
Physiotherapy is always recommended as first line of treatment as research comparing 8-week physio programme made of strength, flexibility and proprioception work versus surgery demonstrated that surgery is no superior to physiotherapy. Pain management strategies will consist of rest, ice, compression and elevation in the short term. An exercise-based approach will consist of exercises to strengthen specific knee muscles. Physiotherapy should also address any impairment in mobility and stability if present.
When to request additional investigations or consider alternative solutions?
Once the diagnosis has been made by the physiotherapist, additional investigations are not required because in most cases they will not inform or change the management program. However, a physiotherapist can recommend an MRI scan for those patients experiencing true knee locking or for those who fail conservative management. Generally, if patients fail to respond to physiotherapy, surgical arthroscopy can be considered.
Degenerative Meniscal Injury
What is it?
Degenerative meniscal injury is a non-traumatic injury of the meniscus, and the onset of pain is gradual and insidious. Pain can occur after a minimal trauma (e.g. kneeling while gardening) or increased loading activity (e.g. a walk significantly longer than usual). Degenerative meniscal injury affects older age groups, and it is often associated with osteoarthritis in the knee. Squatting, kneeling and prolonged walking will often aggravate the knee pain. Pain can be localized on the medial, lateral or posterior aspect of knee. There is often knee swelling and giving way. However, differently than for a traumatic injury, the knee will rarely lock.
What is the management?
Physiotherapy management follows the knee osteoarthritis approach, incorporating education and advice, lifestyle modifications, analgesia and self-management strategies, weight loss, manual therapy techniques and exercise. The best exercise regime will include light aerobic training, local knee muscle strength work, active knee mobility and proprioception exercises. Static, low resistance cycling and aquatic therapy are also effective in reducing pain and improving function. Manual therapy techniques are supported by research if combined with exercise. Footwear and orthotic advice can be suggested by the physiotherapist if appropriate for the patient. Walking aids will be recommended for those individuals with significant pain.
When to request additional investigations or consider alternative solutions?
An MRI scan is indicated to assess the severity of the meniscal damage once physiotherapy has been unsuccessful. However, degenerative meniscal tears should always be considered on the background of osteoarthritis, hence a X-Ray can be suggested to confirm the diagnosis. It is important to remember that there is a poor link between visible changes on X-Ray and osteoarthritis symptoms. Corticosteroid injections are beneficial to reduce pain in case of early-moderate osteoarthritis but not effective for meniscal injuries. Injections will promote pain relief only for few months, their effect tends to reduce the more you use them, and you cannot abuse of injections because, over time, they are shown to increase the amount of joint cartilage degeneration. Therefore, it is always important to use injection as a complementary strategy to manage your pain and always continue with physiotherapy and exercises after you have had the injection. Degenerative meniscal tears can be treated with surgical arthroscopy but, especially for elderly patients with significant degeneration of the knee, there is the concern that more damage can be caused to the joint cartilage during the process. Therefore, often the surgeon will have to evaluate whether knee replacement is better. Knee replacement is generally appropriate for cases of severe pain with functional limitations, when the pain is not controlled with analgesics and the patient has failed physiotherapy.







