Patellofemoral Pain Syndrome (PFPS)
What is PFPS?
Patellofemoral pain syndrome (PFPS) is described as pain arising from the anterior or retropatellar knee region that increases with activities such as running, squatting, stair ambulation, hopping and jumping.
PFPS is a frequent complaint for individuals presenting to physiotherapy or sport medicine clinics. Studies report a high incidence in active populations, with females, particularly young females, affected more often than males. Pain influences short- and long-term prognosis requiring clinicians to deliver early interventions, especially because there is an increasing body of evidence suggesting that PFPS can last from 5-8 years to 20 years in the worst cases.
What causes PFPS?
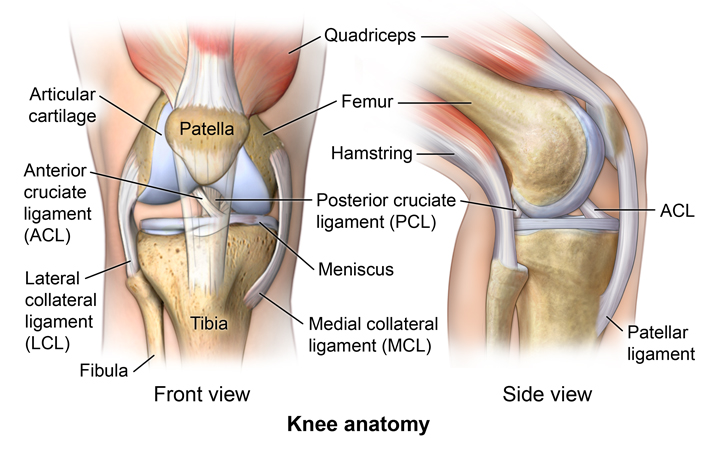
It is generally accepted that PFPS arises from a multifactorial aetiology and that the exact source of symptoms is unclear. Suspected areas that could trigger PFPS are proposed to be all structures of the knee that are innervated, such as:
- Articular cartilage
- Subchondral bone and periosteum
- Vascular tissue
- Synovium and capsule
- Lateral retinaculum
- Fat pad
There are three main theories on the origin of the pain:
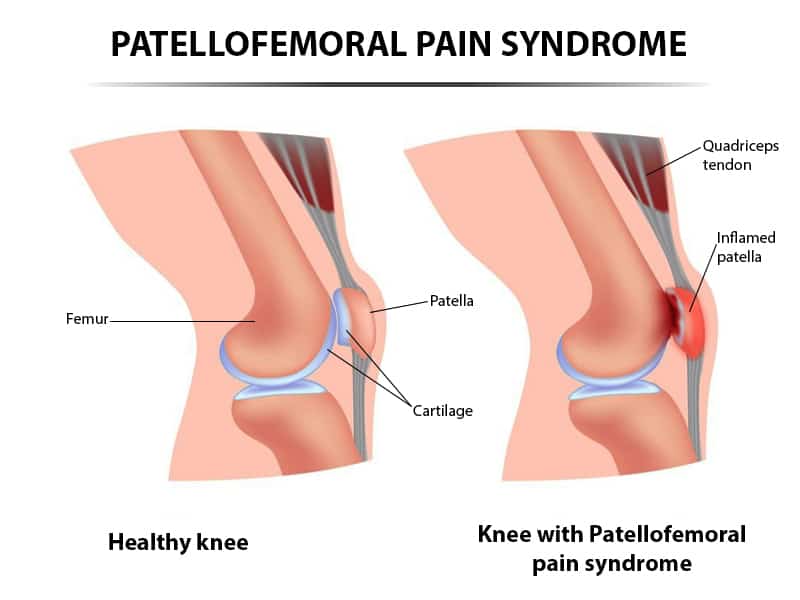
- Patellar malalignment or maltracking
- Overuse
- Trauma
The most accepted theory is the first but, in order to understand it correctly, it is important to introduce the concepts of biomechanics and kinematics. Biomechanics is the application of mechanical laws to the locomotor system of the human body, whereas Kinematics is a sub-area of biomechanics that studies the relative motion between two consecutive segments of the human body. In our case, we shall discuss patellofemoral kinematics as the motions between the two articular surfaces forming this joint, the patella and the femur. It is believed that small changes in the patellofemoral kinematics (in concrete a malalignment or maltracking) create increased shear stress inside the joint thus leading to PFPS development. Patellofemoral kinematics are influenced by how our lower limb moves in the space. Some individuals express abnormal lower limb kinematics altering the dynamic quadriceps angle (Q-angle), which is the angle formed between the quadriceps muscles and the patella tendon.
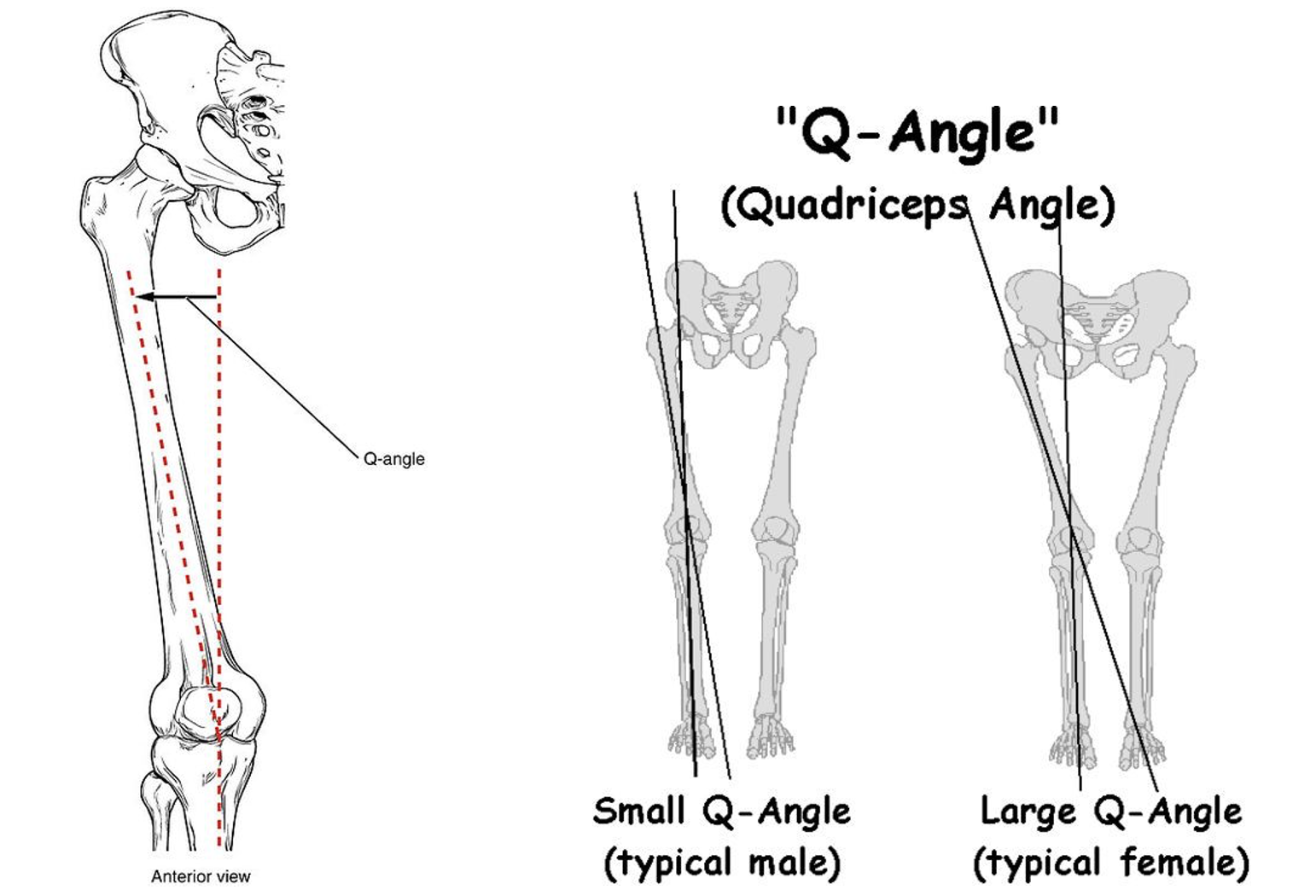
Excessive dynamic Q-angle has been reported in females with PFPS and it is believed to create a lateral patellar displacement, increasing lateral pressures within the patellofemoral joint during anomalous motions of the lower extremity. There are also scientific reviews concluding that certain radiological measures of patella displacement are associated with PFPS. Lower limb kinematic abnormalities that increase the Q-angle are often neglected or missed in individuals playing sports. Some of them include:
- Abnormal foot pronation
- Tibial and femur internal rotations
- Knee abduction/valgus
- Hip adduction and internal rotation
- Contralateral pelvic drop
Physiotherapists have the skills to recognise lower limb kinematic alterations underpinning the problem and, with the right intervention, help restoring normal movements to treat PFPS.
However, it is important to remember that not all individuals suffering from PFPS display abnormal kinematics. This is because PFPS could also be related to overuse or trauma. Overuse refers to the performance of prolonged activities/movements that exceed the physiological capabilities of the patellofemoral joint and associated tissues. For example, in some people excessive amount of running or jumping could irritate the joint thus triggering patellofemoral joint stress and the onset of pain. This could also occur because of direct trauma, like when falling from a bicycle and lending directly to the patella.
What are the main symptoms of PFPS?
Symptoms of PFPS vary greatly among individuals, but the most common are the following:
- Peripatellar pain (diffuse, anterior, retropatellar, anteriomedial or anterolateral)
- Pain during prolonged sitting, running, stair climbing, kneeling, jumping or squatting
- Tenderness on palpation in peripatellar region, compression
- Pseudo-locking (not true locking, meaning that the knee can be manually un-locked)
- Giving way (often occurs on stairs)
- Swelling can be present
- Stiffness (especially after prolonged sitting)
- Crepitus (can also be painful)
- Decreased flexibility of quadriceps, hamstring, gastrocnemius and soleus
- Weakness of quadriceps and gluteal muscles
- Abnormal foot position can be present
Physiotherapy Management
Multimodal physiotherapy can significantly reduce PFPS symptoms. The best multimodal approach incorporates:
- Manual therapy
- Acupuncture
- Strength exercises for quadriceps and gluteal muscles
- Patellar taping
There is strong evidence that this approach is effective at 6 weeks in reducing pain and improving functionality. It will also be important to consider other variables, if present, such as foot posture assessment, stretching and account for psychological barriers that can be present in individuals with fear of pain.